What if it were possible to use microbes to treat infections, outsmarting antibiotic resistance, or even to prevent disease before it starts? Sound too much like science fiction?
Michelle Wright, PhD, RN and assistant professor, doesn’t think so.

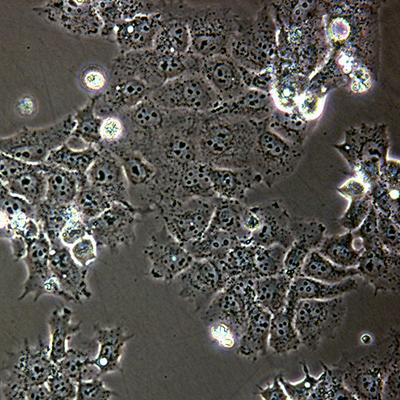
In her lab, she is currently working to identify and modify microbes that grow in and on the human body and turn genetic activity on or off, often causing disease. She is particularly focused on improving women’s vaginal health and reducing pre-term births using a more targeted approach to better understand mechanisms of disease.
In a separate study of human epigenetics, she hopes to discover mechanisms of disease onset and progression of oculophyaryngeal muscular dystrophy to develop treaments to prevent symptoms. She believes it’s possible to develop more successful treatment for chronic diseases by improving our understanding of the interplay among our environmental exposures, microbes, and disease through -omics-based approaches to both basic and clinical research.
Dr. Wright points out that in the past, to better understand how microbes caused disease, researchers had to isolate the microbes, or bacteria, from an infected person, grow the bacteria in the lab and study it directly to determine whether or not it was responsible for making the person sick. But the microbes she studies today can’t be grown in a dish.
“I’m looking at microbes obtained from human samples,” she said. “These microbes might be involved in complex chronic diseases, such as diabetes, or pre-term births; we just don’t have a good understaning of how these microbes contribute to disease or if they show up after people already have the disease.”
Her focus goes back to an earlier interest in DNA methylation, a process by which units of organic compounds attach to a DNA molecule and thereby cause a change in that molecule’s activity.
“Methylation changes how your genes are turned on or off as they respond to stimulus, causing certain segments to be read differently, and can initiate processes that can lead to disease,” she explained. “It can change the expression, what your DNA a is programmed to create, without changing the DNA sequence.”
Methylation is essential for normal development and implicit in understanding health and disease. Picture the way signposts along a trail lead hikers down one path or another and you get a glimpse of how this process makes an impact on cell expression, which is not unlike Dr. Wright’s journey to nursing research.
After obtaining her first degree in biomedical science and chemistry, she worked in groundwater remediation, removing pollution or contaminants from soil and water in the ground to prevent contaminants from entering sources of drinking water. But all along she knew she wanted to improve people’s health more directly and enrolled in a nursing program. After getting a nursing degree, Dr. Wright practiced in emergency departments and a hospital neonatal intensive care unit.
“In hospitals, you start to notice how things work, how all these ‘superbugs,’ or antibiotic resistant microbes, spread,” she said. “I’ve always been interested in microbes, how they get under the skin and make you sick, so I decided to go back into research.”
Upon getting a PhD in nursing from the University of North Dakota, Grand Forks, she returned to an earlier interest in the different microbial populations in pregnant women, particularly group B streptococcus (GBS) and its effect on pre-term births and maternal health.
Explaining that GBS is present in 10 to 30 percent of women often without doing any harm, she said once it shows up in the vagina of pregnant women, it can invade the amniotic cavity and infect an infant’s bloodstream while the women is pregnant or after delivery. GBS is the leading cause of infectious infant mortality, despite antibiotic treatment of mothers during labor to prevent infection of their infants.
When GBS is detected at the time of birth, the mother is given intravenous antibiotics to kill the bacteria and reduce the chance the baby will be infected. Pregnant women are usually tested for GBS via a recto-vaginal swab between the 35th and 37th week, but miscarriages and still births can happen prior to this stage. Dr. Wright believes earlier testing and treatment could lead to improved outcomes for both the mother and child.
Informing her research is the challenge of microbial resistance to antibiotics. The health care community is increasingly worried about the rapid development and spread of “superbugs,” which are bacteria that do not respond to antibiotics. Partly due to natural processes and partly because of the overuse or misuse of antibiotics, many dangerous bacterial strains have become even more threatening by developing resistance to antibiotics.
“Many health care providers and clinics around the world don’t have the ability to quickly and accurately diagnose infectious disease so they throw a broad-spectrum antibiotic at it. We’re now seeing a lot of resistance to those once powerful drugs,” she said. “If we can modify the microbes that grow in and on us, we may be able to develop alternative approaches that will ‘knock out’ pathogens. One day we may be able to grow beneficial microbes that are stronger than the invaders or use what bacteria use to keep bad bacteria at bay and shift individuals into a ‘healthy’ state where they don’t need antibiotics.”
In this way, Dr. Wright is in step with the future of health care, which is moving toward personalized treatment by tracking individual health indicators and focusing on preventive measures more easily integrated into individual lifestyles.
In the meantime, she is excited about the School of Nursing’s collaboration with the Dell Medical School.
“UT Austin has created a very collaborative environment on campus. The Dell Medical School has a cadre of experts in computational statistics and visualization who are also looking at how different microbes can communicate with each other,” she said. “You need a lot of people — a lot of brains! — for this type of research. We’re building a community of researchers who want to work together, who are putting together the building blocks to tackle these important issues.
“We’re not there yet, but we’ll get there. Working together will give us a lot more information that we couldn’t previously get from working in isolation.”
Dr. Wright’s Group B Streptococcus project is supported by a Career Development K01 award from the National Institutes of Health, National Institute of Nursing Research. The award provides support for senior postdoctoral fellows or faculty-level candidates for an intensive, supervised career development experience in the biomedical, behavioral, or clinical sciences leading to research independence.