
Published: January 15, 2021 | Updated: March 9, 2021
On Tuesday, Dec. 16, 2020, Erika Tabke, a faculty member at The University of Texas at Austin School of Nursing, made history by administering the first dose of the COVID-19 vaccine in Central Texas. The day before, UT Health Austin, the clinical practice of Dell Medical School at UT Austin, had received the first shipment of about 3,000 doses, making UT the first health care institution in Central Texas to receive the vaccine.
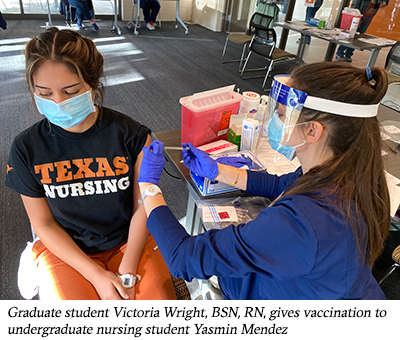
Health care providers, including students and faculty from the UT Austin School of Nursing, Dell Medical School, and the College of Pharmacy, administered the vaccine to frontline health care workers at the UT Health Clinic, and nursing staff and volunteers at the School of Nursing’s Family Wellness Center did the same Dec. 28 through Feb. 5.
In anticipation of being able to provide more people the vaccine through a larger-scale distribution site once larger allocations became available, the university moved vaccine operations to Gregory Gym on Monday, Feb. 8.

Priority for receiving the vaccine is based on guidelines from the Centers for Disease Control and Prevention which puts health care professionals and other high-risk groups at the front of the line. In early January, COVID-19 vaccine began being offered to people aged 65 years and older and those aged 16–64 with underlying health conditions. As of mid-February, more than 34,000 vaccinations have been given.
“Since UT Austin began administering vaccinations, we have served members of the UT Austin community and the UT Health Austin patient population simultaneously,” said Stephanie Morgan, PhD, RN, FNP-BC and co-leader of UT Austin’s COVID Vaccination Task Force. “We will continue our efforts to vaccinate current UT students, staff, and faculty alongside the community as quickly as allowed by vaccine supply to ultimately help our community reach herd immunity.”
The long-awaited vaccine represents hope for not only the individuals receiving it but also the many health care workers who have worked diligently to treat patients in hospitals and clinics during the months since the pandemic was declared. Because of the vaccine, prevention of the transmission of the virus now seems closer than ever, and the beginning of the end of the pandemic could follow soon after.
“As a type 1 diabetic and health care provider, I’m overjoyed to be protecting myself, my patients, my family, and my community,” said graduate student and soon-to-be pediatric nurse practitioner Victoria Wright, BSN, RN, who received a vaccination on Dec. 18.
The smooth rollout of the vaccination clinic belies the herculean effort involved in arranging staffing, storing vaccine at sub-zero degrees, and maintaining COVID-19 pandemic safety guidelines for both individuals seeking the vaccination and health care staff providing it.
Dr. Morgan, director of Practice Innovation, professor of Clinical Nursing, and director of the School of Nursing Wellness Center, described the intense effort to ensure the clinics would be up and ready for the first patients.
“Planning began shortly after receiving a call on Friday, Oct. 30 informing task force members that UT Austin had been designated one of the first sites to receive the vaccine and delivery could be any day following the vaccine’s approval,” she said. “I, along with School of Nursing faculty Dr. Shalonda Horton, Dr. Ana Todd, Dr. Li-Chen Lin, began rehearsing with colleagues from Dell Med and Pharmacy how the clinic would be set up and the flow of patients managed.”
When the vaccine finally arrived on Dec. 14, the team of faculty, alumni, and students was ready and the clinic opened the next day.
“For the benefit of the community, UT Austin is committed to making every effort to distribute vaccines as quickly, equitably and efficiently as possible,” Dr. Morgan said. “Students and other volunteers are very excited to be part of the historic effort and have helped make the clinics run like a well-oiled machine.”

To further help meet this challenge, on Jan. 1, the School of Nursing mobilized the UT Austin Medical Reserve Corps (UTMRC), which was developed by the School after the events of Sept. 11, 2001, and addresses the university’s need to organize and maintain a group of volunteers who are willing and prepared to assist in public health emergencies. Part of the group’s role has been to ensure that clinics have sufficient clinical staff to administer the vaccine but also enough individuals for a variety of tasks, such as checking in patients and manning the observation room, where patients are monitored for adverse reactions to the vaccine.
The vaccination team frequently see tears of joy and report how grateful people are to receive the vaccine and how much it means to them.
“One man at the Family Wellness Clinic was so happy to get the vaccine, even though his daughter had told him not to because she believed we were injecting the actual virus,” one of the volunteers said. “I explained how the vaccine worked and that we were not injecting the virus itself. He told me that his brother had died in Amarillo the week before from COVID and he was so motivated to protect himself.”
An unexpected benefit of the clinics has been the team’s interdisciplinary interactions that have developed seamlessly over the weeks. Team members receive support from each other across the board, and students are able to observe firsthand and participate in the interdisciplinary professional education they have received in the classroom.
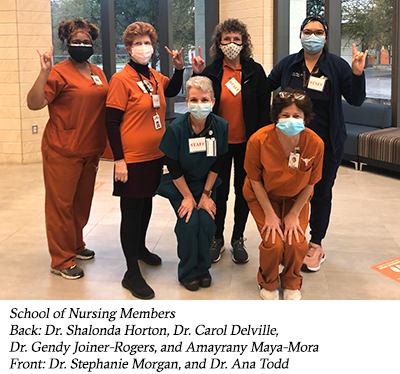
“Our success so far would not be possible without the interprofessional collaboration of medical, pharmacy, and social work faculty, students, and alumni. It’s been beautiful to see everyone work together to make this vaccination effort possible,” Dr. Morgan said. “Everyone still practices within their scope, but where those skills overlap, such as vaccination or mixing the vaccine, the team covers for each other as needed and have shown great concern for any possible burnout. We’ve never done anything like this before, but we’re in for the long haul.”
The hub is currently capable of providing 2,000 vaccinations a day, five days a week, and Dr. Morgan anticipates scaling up to 4,000 when larger shipments of the vaccine are received. To accomplish this, growing numbers of volunteers will be needed to facilitate the pre-check and check-in areas.
“Nurse leadership, such as that exhibited by Dr. Morgan, Dr. Horton, Dr. Todd, Dr. Lin, and Dr. Gendy Joiner-Rogers and others, should come as no surprise to anyone,” said Alexa Stuifbergen, dean of the School of Nursing. “Since the era of Florence Nightingale, nurses have fearlessly faced deadly illnesses and disease. Today, in the midst of great personal risk, our team is making a wholehearted effort to eradicate COVID-19, whether by vaccination, treatment or research. I can’t say enough about how tirelessly so many of our faculty have worked. They have been at the clinics five, sometimes seven, days a week — evenings and through the holiday break — in addition to their regular jobs. To call them ‘heroes’ is no exaggeration; it is simply true.”